Background
Oral anticoagulants are the recommended therapy for prophylaxis and treatment of venous thromboembolism and for stroke prevention among patients with non-valvular atrial fibrillation. Given their widespread use, clinicians must balance efficacy and anticoagulation associated bleeding risks. Intracranial hemorrhage (ICH) has been the most feared complication, as this form of bleeding has been associated with the greatest morbidity and mortality. Clinical trials suggest a lower incidence of ICH among patients prescribed the direct oral anticoagulants (DOACs) compared with vitamin K antagonists (VKAs). While reassuring, the clinical impact on functional outcomes once an anticoagulant-associated ICH does occur is needed. The aim of this study was to evaluate the role of anticoagulation use on in-hospital mortality rates, and functional outcomes among survivors presenting with ICH.
Methods
In this study, we present data from a retrospective chart review of patients who presented to The Ottawa Hospital, Ottawa, Canada with ICH between January 2016 and December 2017. Patients were identified from the Ottawa Hospital Data Warehouse using ICD-10 codes. Patient demographics, type of anticoagulant/antiplatelet agent and indication for therapy were collected. The primary outcome was in-hospital mortality rates among patients prescribed oral anticoagulants compared with those not anticoagulated or on antiplatelet therapy. A secondary outcome was functional assessment of survivors at hospital discharge using the modified Rankin Scale (mRS), a validated tool used widely in contemporary stroke research to measure the degree of disability after a neurological event.
Results
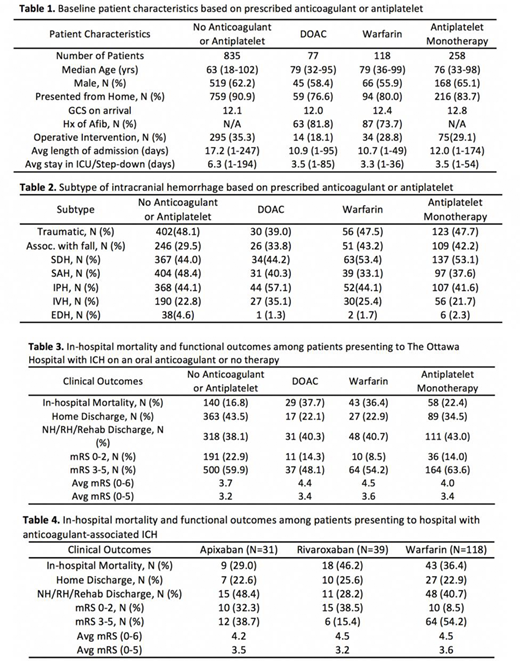
1457 patients were identified in the Ottawa Hospital Data and 1331 patients with ICH were confirmed by manual review. 195 patients were on an oral anticoagulant, and the primary indication for anticoagulation was atrial fibrillation (Table 1). Intraparenchymal bleeding was most common among patients on DOACs, while patients on warfarin tended to have more subdural hematomas (Table 2). In-hospital mortality was 37.7% in DOAC-related ICH, 36.4% in warfarin-related ICH and 16.8% in patients not on an antithrombotic therapy. The average modified Rankin Scale (excluding death as a competing factor) at the time of discharge was 3.4 in DOAC-related ICH, 3.6 in warfarin-related ICH and 3.2 in patients not on an anticoagulant or antiplatelet (Table 3). The majority of patients with a DOAC-related ICH were on Apixaban or Rivaroxaban. The in-hospital mortality for patients on Apixaban (N=31) and Rivaroxaban (N=39) was 29.0% and 46.2%, respectively (Table 4).
Conclusions
In this cohort of patients presenting with ICH to a large academic hospital, the in-hospital mortality rate was higher in patients receiving oral anticoagulation compared to those not on anticoagulants. DOAC-related ICH tended to have similar in-hospital mortality when compared to warfarin; however, among survivors, functional outcomes at discharge tended to be more favourable in the DOAC cohort. Although the DOACs are reported in the literature to have an overall lower incidence of ICH, prospective studies are needed to understand the clinical impact when a bleeding event does occur.
Castellucci:Servier: Honoraria; Bayer: Honoraria; BMS-Pfizer: Honoraria; LEO Pharma: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal